Shin pain with exercise? It could be Compartment Syndrome

What is Compartment Syndrome?
Compartment syndrome is one of the 3 conditions under the “shin splints” umbrella – the others being Tibial Stress Reaction/Fracture and Tibialis Posterior Tendinopathy. Although it is the least common of the 3, compartment syndrome can be very debilitating.
Anatomy
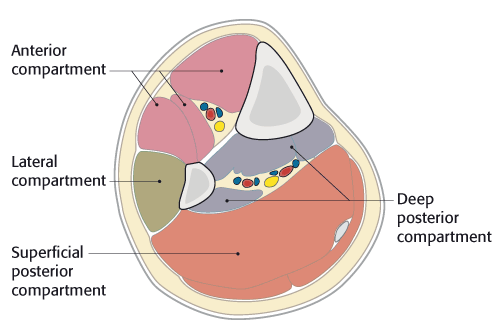
The lower leg is made up of groups of muscles that are surrounded by what is known as fascia (an expandable, ‘glad wrap’ like covering). The fascia separates these groups of muscles into four compartments:
- Anterior
- Lateral
- Superficial posterior
- Deep posterior
Compartment syndrome is most common in the anterior compartment
How do I know if I have it?
Symptoms can include any of the following in the lower leg every time you exercise:
- Tightness
- Burning
- Pressure
- Cramping
- Pain
The most common areas for these symptoms is the calves and shins.
In most cases you have no pain at rest but with exercise the pain comes on, usually after a set period of time. If you continue to exercise the pain gets worse and usually completely relieved with rest.
Some more uncommon symptoms may include:
- Sudden fatigue on the top of foot/ankle
- Numbness between the big toe and second toe
- Drop foot
What causes it?
When the muscle groups are overused, the fascia starts to lose elasticity and thicken. During exercise the muscles increase in size meaning the thickened fascia begins to cause compression between the muscles. Compartment syndrome normally becomes evident with an increase in training load or activity as the muscle volume increases and therefore pressure inside the compartments increase.
After exercise the pressure would normally resolve after ~5mins. In the case of compartment syndrome, it takes longer to reduce post-exercise. Due to this increased pressure, there is a restriction of blood flow to the muscle and therefore reduced oxygen getting to the muscle – this creates the pain. In some severe cases nerve function can be affected causing pins and needles. Typically, symptoms reduce after several minutes of rest, however an ache can remain for up to 30minutes.
Diagnosis
The only definitive diagnosis is via compartment pressure testing, where a catheter is inserted into the compartment to take pressure readings whilst the patient is exercising.
Treatment
Compartment pressure testing is not required in all cases, with physiotherapists well equipped to assess and correct the many other predisposing factors (excessive muscle tension and poor foot biomechanics are the common culprits). Treatment of the predisposing factors will often resolve the problem, however severe/persistent cases can require surgery.
Your Physiotherapist can use a range of treatment tools to:
- Reduce your pain
- Advise you on any necessary modifications to activity/training loads
- Restoring normal joint range of movement, muscle length and fascial flexibility
- Restoring muscle control and strength
- Get you back to full function
- Prevent reoccurrence
If you are experiencing shin pain, make sure you see your Physiotherapist for a thorough assessment.
Physiotherapist